An Everyday DNA blog article
 By: Sarah Sharman, PhD, Science Writer
By: Sarah Sharman, PhD, Science Writer
Did you know that chemotherapy was born out of the trenches of World War I? While working on an antidote for mustard gas, a nasty chemical weapon used by both sides during the war, scientists discovered that the agent was damaging the soldiers’ bone marrow, halting its ability to make new blood cells. This gave scientists an idea: since cancer cells and bone marrow cells both replicate so rapidly, can we create safer agents similar to mustard gas to kill cancer cells?
By the end of World War II, after many years of research and trials, scientists had developed the first chemotherapeutic agent. Today, there are more than one hundred different chemotherapies available for use. This article will briefly discuss how chemotherapy works and what happens when it stops working.
How does chemotherapy work?
Traditional chemotherapies are cytotoxic compounds, meaning they kill living cells. Although they do most of their damage to rapidly dividing cells, like cancer cells, chemotherapy can still affect healthy cells which leads to some of the common side effects of the drugs.
 Chemotherapy drugs target cancer cells at different phases of the cell cycle to stop their characteristic, uncontrolled rapid growth. Some types of chemotherapy drugs keep cancer cells from multiplying by damaging their DNA. Other types interfere with DNA and RNA by acting as a substitute for the normal building blocks of RNA and DNA. A third type of chemotherapy interferes with enzymes involved in copying DNA during the cell cycle.
Chemotherapy drugs target cancer cells at different phases of the cell cycle to stop their characteristic, uncontrolled rapid growth. Some types of chemotherapy drugs keep cancer cells from multiplying by damaging their DNA. Other types interfere with DNA and RNA by acting as a substitute for the normal building blocks of RNA and DNA. A third type of chemotherapy interferes with enzymes involved in copying DNA during the cell cycle.
What is chemotherapy resistance?
Chemotherapy is used as standard treatment (usually in combination with surgery) for many cancer patients. While a patient may respond positively to treatment for weeks, months, or years, they may hit a wall where the treatment is no longer working and the tumor begins to grow again. This devastating phenomenon referred to as chemotherapy resistance occurs for a variety of reasons that are either intrinsic to the cancer cells, acquired during the treatment, or a combination of both.
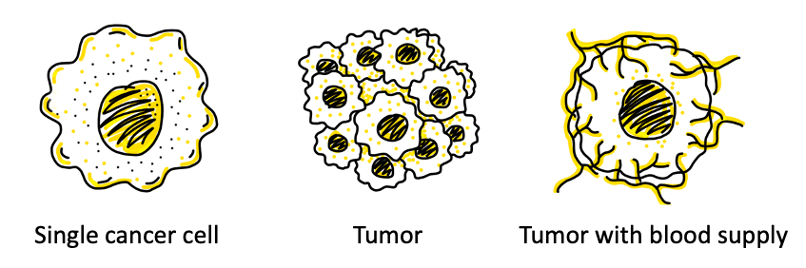
Tumors are heterogenous, meaning that not all of the cells in the tumor are genetically identical. In addition to cancer cells, tumors also consist of immune cells, blood vessels, fibroblasts, and other cells and components, called the tumor microenvironment, that interact with the cancer cells and influence the way they react to treatments.
When this mixed bag of cancer cells and the microenvironment is exposed to chemotherapy, many cells will be killed. But sometimes a small subset of cells survives the chemotherapy and continues growing. This type of resistance that occurs in cells upon the first exposure to chemotherapy is called intrinsic resistance.
Mechanisms of resistance: genetic factors
In the face of chemotherapy, cancer cells can also acquire resistance and switch on protective shields by developing new mutations or reproducing protective genes. If we picture cancer as a car driving down the road, roadblocks like the immune system and cancer treatments can slow it down or block its way. A dominant mutation, called the driver mutation, allows the cancer to initially thrive and survive, avoiding the roadblocks.
Researchers and physicians aim to shut down the cancer by identifying and targeting driver mutations. However, just like in a real car, a passenger, or secondary mutation, can take over, allowing the cancer to survive and grow again. When cancer adapts like this, resistance occurs and a new treatment must be initiated. In this way, cancer cells can acquire resistance to many types of chemotherapy, called multiple drug resistance.
Mechanisms of resistance: transport pumps
 For chemotherapy to be effective, it must reach and enter into the cancer cell it is trying to destroy. Some cancer cells protect themselves from chemotherapeutic damage by keeping the drug out of the cell so it cannot initiate cell death protocols. In many cells, biological molecules, drugs, and other chemicals enter the cell through special channels called transport pumps. Some cancer cells find ways to reduce the expression of transport pumps on the cell membrane, meaning less drug is able to enter into the cell.
For chemotherapy to be effective, it must reach and enter into the cancer cell it is trying to destroy. Some cancer cells protect themselves from chemotherapeutic damage by keeping the drug out of the cell so it cannot initiate cell death protocols. In many cells, biological molecules, drugs, and other chemicals enter the cell through special channels called transport pumps. Some cancer cells find ways to reduce the expression of transport pumps on the cell membrane, meaning less drug is able to enter into the cell.
Cancer cells can also hijack the cellular transport pumps and reprogram them to pump the drug back out of the cell before it can cause damage to the cell. Scientists are developing drugs that inhibit transport pumps to allow chemotherapies to remain inside cells longer, giving them more time to work.
Mechanisms of resistance: DNA repair
Many chemotherapies cause damage to DNA within cancer cells, which triggers a process of programmed cell death called apoptosis. Some cancer cells enhance or activate DNA repair pathways so that they fix the DNA damage induced by the chemotherapy before the cell has had the time to initiate apoptosis. In some cases, repaired cancer cells become more resistant to the chemotherapy.
What are scientists doing to combat chemotherapy resistance?
As we’ve described above, cancer cells are masters of adaptation, adjusting their molecular and cellular characteristics to survive. Many scientists are focused on solving the problem of chemotherapy resistance by identifying ways to target the mechanisms of cancer chemotherapy resistance like genetic mutations, drug transport, and DNA repair pathways.
The HudsonAlpha Institute for Biotechnology’s cancer programs are committed to the goal of using genomic science and state-of-the-art technology to find new breakthroughs in cancer research and treatment. The lab of Faculty Investigator Sara Cooper, PhD, is focused on linking patients with their own personalized treatment plan based upon their tumor’s own genetic fingerprint.
Cooper’s lab is using genome-wide CRISPR screening methods to identify genes associated with chemotherapy resistance in pancreatic and ovarian cancer. The CRISPR screen provides a promising new tool to predict a patient’s likelihood of developing resistance to common treatments, and help make informed treatment decisions. In addition, some of the new targets that are identified using the CRISPR screen are being used to identify and produce new therapeutics for cancer treatment. To hear Dr. Cooper talk more about her research, watch this episode of Genomics and Java.