May 3, 2021 (Huntsville, Ala.) – HudsonAlpha Institute for Biotechnology Junior Fellow Le Su, PhD has been studying the cancer synovial sarcoma for over a decade. In a new commentary published April 25, 2021 in Molecular & Cellular Oncology, Su and coauthor Christina Cooley, a research associate in his lab, discuss the progress and exciting discoveries that Su’s lab and the synovial sarcoma research community have made toward a treatment for this rare disease.
Synovial sarcoma: signs, symptoms, diagnosis, and treatment
Synovial sarcoma is a rare and aggressive form of soft tissue cancer. The tumors commonly arise in the soft tissues near the large joints of the arms and legs. It generally affects children and young adults under the age of 30. Synovial sarcoma occurs in one to three people per million, with about 800 new cases diagnosed in the United States each year.
The tumors grow slowly and often go unnoticed until they develop into a mass or cause swelling and pain near the affected area. As such, metastatic disease is common in synovial sarcoma patients and usually fatal.
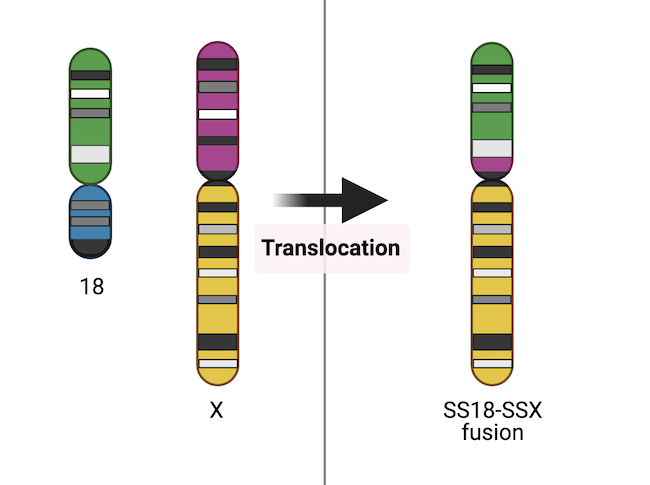
While the exact cause of synovial sarcoma is not well understood, genetics is thought to play a role. Almost all synovial sarcomas carry a common genetic abnormality—a fusion gene called SS18-SSX. Fusion genes are produced by a phenomenon called chromosome translocation where part of one chromosome breaks off and fuses to part of another chromosome.
In the case of SS18-SSX, the SS18 gene of chromosome 18 breaks off and fuses to one of three genes on the X chromosome: SSX1, SSX2, or SSX4. Studies have shown that the protein product of the SS18-SSX fusion gene functions as an oncoprotein, meaning it can transform a healthy cell into a cancer cell.
Currently, surgery is the mainstay of synovial sarcoma treatment, rendering many individuals disease-free. In cases in which the tumor is hard to access or remove completely, radiotherapy may also be used to reduce the risk of leaving cancerous cells behind. Chemotherapy is often combined with surgery and radiotherapy in advanced stage or metastatic disease. There remains a need for a treatment that targets the molecular root of synovial sarcoma.
Potential new targets for treating synovial sarcoma
The newly published Molecular & Cellular Oncology commentary chronicles Su’s journey to discovering a potential treatment for synovial sarcoma, which started during his graduate training. While pursuing his PhD at the University of British Columbia in Canada, Su was involved in research that led to breakthroughs that defined a critical role for SS18-SSX in dysregulation of tumor suppressor pathways which act to inhibit cell proliferation and tumor development.
“During my time in graduate school, we learned more about how the fusion protein works, and we narrowed in on a pathway that might be carrying out the actions,” says Su. “Once I set up my lab at HudsonAlpha we began asking the next question: now that we know how this protein is functioning, can we reverse its effects?”
Su thought ‘what if we ignore the genetic mutation itself and just try to get rid of the oncoprotein product that is wreaking so much havoc in these individuals.’ He turned to a pathway that our bodies naturally use to recycle and rid itself of unneeded or damaged proteins, called the protein degradation pathway, or ubiquitin-proteasome system (UPS).
In the UPS, proteins are tagged with a molecule called ubiquitin, marking them for degradation. The tagged proteins are dragged to a cellular structure called the proteasome where they are destroyed.
Su and his colleagues discovered a class of drugs called histone deacetylase (HDAC) inhibitors that were potent killers of synovial sarcoma cells in tissue culture and also stimulated the process of protein degradation. HDAC inhibitors have a long history in psychiatry and neurology as mood stabilizers and anti-epileptics but have more recently been investigated as treatments for cancers in addition to parasitic and inflammatory diseases.
Their study, which was published in iScience in 2019, presented promising results that support the use of HDAC inhibitors to treat synovial sarcoma. Su and his team reported that HDAC inhibition facilitates proteasomal degradation of the SS18-SSX fusion protein. They also found that a protein called MULE marks SS18-SSX for degradation with a ubiquitin molecule.
“The progress that we have made characterizing the molecular effect of HDAC inhibitors on synovial sarcoma is exciting,” says Su. “Even more exciting is that we have teamed up with sarcoma specialists across the world to facilitate clinical trials with these drugs. It is always a great feeling when your research transitions from the lab to the clinic to potentially help many patients.”
For first author Christina Cooley, the newly published commentary means so much more than just an opportunity to share new findings in the synovial sarcoma field. This represents Cooley’s first publication in a scientific journal and fulfills one of her career goals.
She first caught the research bug in high school and decided to participate in HudsonAlpha’s BioTrain internship program the summer of her junior year. After receiving her bachelor’s degree from the University of Alabama in Birmingham, Cooley returned to HudsonAlpha to further her lab experience as a research associate in Su’s lab.
“I am a very hands-on person and love seeing my knowledge from classes put into real world applications,” says Cooley. “Our research into synovial sarcoma is very fulfilling for me because I get to broaden that knowledge and my laboratory skills in a terrific environment while knowing my work has a direct and beneficial impact.”
Looking to other fusion gene associated cancers
Su’s lab is following the same vein to study other types of fusion gene-associated sarcomas, like CIC-DUX4 sarcoma. As in the synovial sarcoma story, scientists know the mutation in CIC-DUX4 sarcoma, and they know how the mutation works. Using the same pipeline, Su wants to determine how to target the proteins for degradation and remove them from the patient’s body.
The team is also very interested in pushing HDAC inhibitors further into the protein world. Historically, HDAC inhibitors have been used for their role in blocking the action of a molecule called histone deacetylase which helps regulate gene expression by wrapping DNA molecules more tightly around a histone. With these sarcoma studies, Su has now begun looking at the effectiveness of HDAC inhibitors in targeting proteins and protein function.
About HudsonAlpha: HudsonAlpha Institute for Biotechnology is a nonprofit institute dedicated to developing and applying scientific advances to health, agriculture, learning, and commercialization. Opened in 2008, HudsonAlpha’s vision is to leverage the synergy between discovery, education, medicine, and economic development in genomic sciences to improve the human condition around the globe. The HudsonAlpha biotechnology campus consists of 152 acres nestled within Cummings Research Park, the nation’s second largest research park. The state-of-the-art facilities co-locate nonprofit scientific researchers with entrepreneurs and educators. HudsonAlpha has become a national and international leader in genetics and genomics research and biotech education and fosters more than 40 diverse biotech companies on campus. To learn more about HudsonAlpha, visit hudsonalpha.org.