Summary
Researchers at HudsonAlpha and UAB release the largest published study to examine epigenetic risk pathways for lupus.
Highlights
-
Study included about 100 patients, divided between those diagnosed with lupus and a control group of patients without autoimmune disease.
-
Researchers observed diminished DNA methylation around genes that respond to interferon, a potent protein involved in viral infections
-
Findings suggest lupus patients are hypersensitive to interferon.
Study of the epigenome searches for disease triggers
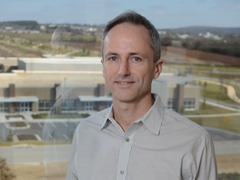
Using genome-wide analyses, researchers at the HudsonAlpha Institute for Biotechnology along with clinical and research partners at the University of Alabama at Birmingham, have released the largest published study that examines epigenetic risk pathways for lupus. Lupus is an autoimmune disease that occurs primarily in women and is known to have both genetic and epigenetic causes. The disease may affect various parts of the body, especially the skin, joints, blood and kidneys.
Researchers examined DNA methylation, an epigenetic modification to the genome that modulates gene expression. The study included about 100 patients, divided between those diagnosed with lupus and a control group of patients without autoimmune disease. Among the lupus patients, researchers observed methylation was diminished around genes that respond to interferon, a potent protein involved in viral infections. This reduction, called hypomethylation, suggests lupus patients are hypersensitive to interferon.
“That wasn’t particularly surprising,” said Devin Absher, Ph.D., faculty investigator at HudsonAlpha, “but what’s novel is the hypomethylation didn’t fluctuate; that is, it remained consistent, even in patients with quiescent disease.” Absher worked closely with Robert Kimberly, M.D., UAB School of Medicine Division of Clinical Immunology and Rheumatology.
A characteristic of lupus includes periodic flares typically involving increased joint inflammation plus spikes among more than a dozen other symptoms.
The study found the consistent hypomethylation levels to be remarkable because circulating interferon and the expression of associated genes are known to increase during disease flares, but return to normal during a quiet phase. Hypersensitivity to interferon, therefore, appears consistent across all phases of the disease, and may explain why the disease is chronic and persistent.
Notably, researchers looked at three immune cell types: T-cells, B-cells and monocytes. “Each was studied independent of the other types,” Absher said. Findings revealed widespread changes among all cell types in lupus patients, “far more than anticipated,” according to Absher, with highest levels of change occurring around genes involved in interferon response.
In a second phase of the study involving a subset of patients, researchers sorted T-cells into subsets that might have been likely to be the source of the observed hypomethylation. “We found no enrichment, no differences among these types,” said Absher.
“We need more experiments to understand what cell types specifically carry this aberrant methylation and where they come from,” Absher said. “Are they early progenitor cells that are giving rise to hypersensitized immune cells throughout a lupus patient’s life or are there constant hypersensitization steps happening in all immune system cells because of some constant stimulus?”
Looking forward, Absher hopes to conduct a thorough analysis of additional subsets of the immune system to determine which cell types carry these trends.
The paper Genome-wide DNA Methylation Analysis of Systemic Lupus Erythematosus Reveals Persistent Hypomethylation of Interferon Genes and Compositional Changes to CD4+ T-cell Populations is published in PLOS Genetics on 8 August 2013. The paper may be found here.
Lupus has been studied at a genetic level for several years, yielding the identity of many risk factors. Fewer studies have been conducted that focus on epigenetic risk factors.
About HudsonAlpha
The HudsonAlpha Institute for Biotechnology in Huntsville, Alabama, is the cornerstone of the Cummings Research Park Biotechnology Campus. The campus hosts a synergistic cluster of life sciences talent – science, education and business professionals – that promises collaborative innovation to turn knowledge and ideas into commercial products and services for improving human health and strengthening Alabama’s progressively diverse economy. The non-profit institute is housed in a state-of-the-art, 270,000 square-ft. facility strategically located in the nation’s second largest research park. HudsonAlpha has a three-fold mission of genomic research, economic development and educational outreach.